
The healthcare industry has reached a critical inflection point. Data is no longer a byproduct of patient care—it's the foundation that determines the sustainability of an organization. Thus, for healthcare boards and C-suite executives - data governance has evolved from an IT department responsibility to a strategic imperative that directly impacts patient safety, regulatory compliance, and organizational survival.
The question isn't whether your organization needs robust data governance. It's whether your board is prepared to lead this transformation before regulatory penalties, security breaches, or clinical errors force your hand.
Healthcare's Most Valued Asset: Trusted, Governed Data
As per a World Economic Forum report, “Healthcare organizations generate approximately 50 petabytes of data annually”—a figure that doubles every 73 days. This exponential growth encompasses electronic health records (EHRs), medical imaging, genomic data, wearable device inputs, and AI-generated insights. Yet without governance creates risks- not value.
Consider the modern healthcare ecosystem: EHRs store patient histories across multiple systems, AI algorithms analyze diagnostic images in real-time, patient portals provide 24/7 access to medical information, and telemedicine platforms collect biometric data during virtual consultations. Each touchpoint generates data used in life-critical decisions.
When this data lacks proper governance, it becomes a liability rather than an asset. Inconsistent formatting across systems leads to diagnostic errors. Incomplete patient records result in adverse drug interactions. Outdated information triggers unnecessary procedures. These aren't hypothetical scenarios—they're daily realities in healthcare organizations that treat data governance as a secondary concern.
The board's role has fundamentally shifted. Data governance decisions now directly impact patient outcomes, regulatory standing, and competitive positioning. Organizations that govern data strategically gain the ability to deploy AI safely, personalize patient care, and respond rapidly to public health challenges. Those that don't face mounting risks that threaten their core mission.
The Risks Are Rising — and the Stakes Are Higher in Healthcare
The healthcare industry faces a unique risk profile that makes data governance failures particularly consequential. Unlike other industries where data breaches primarily impact financial or operational systems, healthcare breaches directly threaten patient safety and organizational credibility.
Cybersecurity Threats Target Healthcare Data
Healthcare organizations experience cyberattacks at rates 2.5 times higher than other industries. Ransomware attacks have paralyzed major health systems, forcing hospitals to revert to paper records and delay critical procedures. The 2022 attack on CommonSpirit Health affected over 100 facilities, disrupting patient care for weeks and costing an estimated $160 million in recovery efforts.
These attacks succeed because healthcare data governance often prioritizes accessibility over security. Clinical systems require immediate data access for emergency care, creating inherent tensions between usability and protection. Without strategic governance frameworks, organizations struggle to balance these competing demands, leaving vulnerabilities that attackers exploit.
Regulatory Compliance Carries Escalating Penalties
Healthcare operates under some of the most stringent data protection regulations globally. HIPAA violations now carry penalties up to $1.5 million per incident, while HITECH Act violations can reach $2 million. The EU's GDPR imposes fines up to 4% of annual global revenue for healthcare organizations serving European patients.
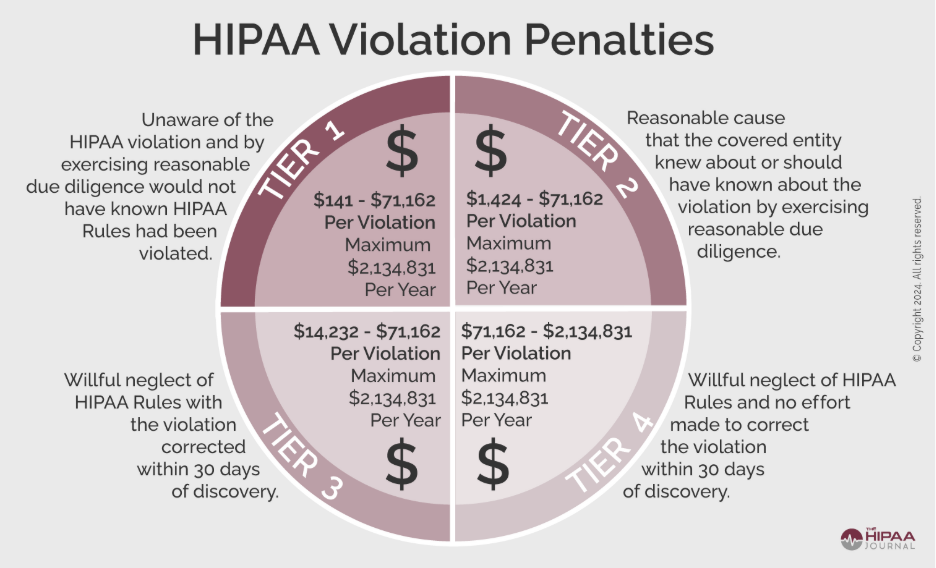
Credits: The HIPAA Journal
Recent enforcement actions demonstrate regulators' increasing focus on data governance failures. The Office for Civil Rights has already issued more than $6 million in HIPAA fines in 2025, with many penalties specifically targeting inadequate data governance practices rather than isolated breaches. Organizations face scrutiny not just for what happened, but for their failure to implement proper governance frameworks that could have prevented incidents.
Clinical Decision-Making Depends on Data Integrity
When patient records are incomplete, outdated, or inconsistent across systems, the risk isn’t just operational—it’s clinical. Misdiagnoses, treatment delays, and even adverse outcomes often trace back to unreliable data. A robust data governance framework ensures the accuracy, consistency, and accessibility of patient data across departments and platforms—empowering physicians to act with confidence and speed.
What Strategic Healthcare Data Governance Looks Like
Effective healthcare data governance requires organizational structures that bridge clinical, technical, and regulatory domains. This isn't about implementing new technology—it's about creating accountability frameworks that ensure data serves patients safely and effectively.
Data Councils with Cross-Functional Leadership
Strategic data governance in healthcare begins with establishing data councils that include medical staff, IT leadership, legal counsel, and quality officers. Cross-functional data councils with authority—not ceremony. They must have executive authority to make binding decisions about data standards, access controls, and quality metrics.
The most effective data councils operate with clear mandates: clinical leaders define data quality standards based on patient care requirements, IT teams implement technical controls that support those standards, and legal counsel ensures compliance with regulatory frameworks. This collaborative approach prevents the siloed thinking that often undermines governance initiatives.
Standardized Clinical Coding and Metadata
Healthcare data governance requires standardized approaches to clinical coding and metadata management. Organizations must implement consistent terminologies across all systems—using standards like SNOMED CT for clinical terms, LOINC for laboratory data, and RxNorm for medications. This standardization enables data sharing across departments and systems while maintaining clinical accuracy.
Metadata governance proves equally critical. Clinical data without proper context becomes meaningless or dangerous. Governance frameworks must ensure that every data element includes information about its source, collection method, validation status, and clinical significance. This metadata enables clinical teams to assess data reliability and make informed decisions about patient care.
Auditable Lineage from Source to Use
Healthcare data governance demands complete visibility into data lineage—the ability to trace any data element from its original source through all transformations to its final use. This requirement becomes especially critical when AI systems analyze patient data for diagnostic or treatment recommendations.
Auditable lineage enables organizations to identify data quality issues, validate AI model inputs, and respond to regulatory inquiries. When clinical decisions are questioned, governance frameworks must provide clear documentation of the data sources, processing steps, and validation checks that inform those decisions.
Governance as an Enabler for AI and Patient-Centered Care
Rather than constraining innovation, strategic data governance enables healthcare organizations to deploy advanced technologies safely and effectively. Governance frameworks create the foundation for AI implementations that enhance rather than endanger patient care.
Clean Data Powers Precision Medicine
Precision medicine requires integrated data from multiple sources—genetic information, clinical histories, lifestyle factors, and treatment responses. Governance frameworks that standardize data collection and ensure quality enable organizations to identify patterns that inform personalized treatment approaches.
Consider oncology care, where treatment decisions increasingly depend on genetic markers, treatment histories, and population health data. Governance frameworks that ensure data accuracy and completeness enable oncologists to select targeted therapies with confidence. Without governance, the same data becomes unreliable for clinical decision-making and potentially dangerous for patient care.
Governance Unlocks Safe, Scalable AI Implementation
AI systems in healthcare require exceptional data quality standards because errors can directly harm patients. Governance frameworks that validate data inputs, monitor model performance, and maintain audit trails enable organizations to deploy AI safely across diagnostic, treatment, and operational workflows.
Healthcare organizations that implement strategic governance frameworks position themselves to benefit from AI advances while maintaining patient safety. Those that don't face mounting risks as AI becomes integral to clinical care delivery.
Boardroom Questions to Ask Your Data Leaders
Data governance isn’t just an IT problem—it’s a boardroom priority. Here are key questions to help you stay in the driver’s seat:
Incident Response and Recovery Capabilities
- How quickly can we respond to a data breach—and can we keep patient care running during one?
- Who’s in charge when things go wrong, and how do we keep patients, regulators, and staff informed?
AI Readiness and Data Quality
- Is our data good enough for safe, reliable AI use? What checks are in place to keep it clean and unbiased?
- How do we double-check AI recommendations—and who’s responsible if something goes off track?
Executive Accountability and Ownership
- Who’s accountable for clinical data quality at the top—and how do we measure their impact?
- Are we investing enough in data governance? And how do we decide what gets priority?
The Path Forward
Healthcare data governance has evolved beyond technical implementation to become a strategic imperative requiring board-level leadership. Organizations that recognize this shift and act accordingly will gain competitive advantages through safer AI deployment, enhanced patient care, and regulatory compliance. Those that continue treating data governance as an IT concern face mounting risks that threaten their core mission.
This is not just about rules and checklists. It’s about building a resilient, intelligent, patient-first healthcare organization. One that’s ready for tomorrow, not stuck fixing yesterday’s mistakes.
Put data governance where it belongs: in the boardroom.
CTA: Let’s talk.
