Our health and social care system is incredibly complex. In order to address system-wide issues, we need to take a system-wide approach to the design and delivery of solutions. The creation of Integrated Care Systems indicates a move towards a joined-up approach to health and social care, requiring a concerted effort to apply system-level thinking to the problems facing the NHS.

Joining up and digitising systems are themes common across NHS, with more IT spending going towards digital rather than legacy IT system spending. Applying a service design approach is instrumental in solving complex problems such as these. Digital service design gives you methodologies, tools and techniques to tackle systemic issues. Let’s look at how.
What is an ICS?
Integrated Care Systems (ICSs) are partnerships of health and care organisations that plan, coordinate and commission health and care services across large geographical areas. As of July 2022, when the 2022 Health and Care Act established ICSs as a statutory entity, there were 42 ICSs across England.
They aim to bring organisations together to better meet the needs of patients and staff, by working in a joined-up way. This means creating partnerships between primary and secondary care, social care, mental health and community health services, as well as local authorities, and voluntary and community organisations. ICSs create networks through which to share resources and learnings. They also enable closer working with local people and community organisations, to provide a wider range of services.
You can find out more about the ICS structure: The King’s Fund - How Does the NHS in England Work?
What challenges is the NHS addressing through the creation of ICSs?
At a high level, the NHS is seeking to integrate services to:
- improve population health
- reduce inequalities in health outcomes
- increase efficiency so there is more value for money in service provision
Bringing together organisations enables interoperability and the exchange of data. This, in turn, helps commissioners make better-informed decisions on where to invest resources.
This reform has brought in a new partnership and delivery structures. But it also ushers in a new approach to ways of working within the health and care system. It heralds a move away from competition and organisational autonomy and promotes a collaborative model that encourages partnership working with holistic development and integrated services.
What is digital service design?
Defining services: people, process, technology
The definition of a “service” is deceptively simple. As Lou Downe, former Head of Design for Government, puts it, “A service is something that helps someone to do something.” Wrapped up in this seemingly simple goal, is a wealth of complexity. Particularly when we are talking about delivering services in healthcare. Downe continues: “The parts of that service might be provided by a number of different organisations, but to a user, service is one continuous set of actions towards that end goal, regardless of who is providing it.” Service design is about bringing together a wide range of stakeholders, organisations, technologies, policies and processes to enable users to reach that end goal.
To put that into perspective, in a single acute hospital there could be up to 140 different IT systems that keep the organisation running. Things from appointment booking systems to data transfer protocols, internal staff software, specialist tools for running diagnostic tests, or programs which enable the processing of lab results.
Using this interconnected web of systems are users. Those users could be from hugely diverse backgrounds. They will undoubtedly have different needs, goals, capabilities and barriers. They have different motivations, and different tasks they need to complete as part of their job role, in order to get the care they need. In our acute hospital example, these could be patients, clinicians, lab technicians, administrative support staff, policy-makers, or commissioners.
Underpinning all of this are policies, processes and procedures. To use an analogy, our different types of users are operating differently, depending on what it is they need to achieve. These users are not always going to perfectly align.
How should we apply service design thinking to complex systems?
So how do we orchestrate such a complex system? One with such a wide variety of people, processes and technologies? We can use a systemic, service design approach to understand the inner workings of the current system. We then take this rich knowledge of the current state of play, design interventions to make improvements, and ultimately reach our overall intended outcomes. In reality, this design intervention could take any number of shapes.
It might look like re-designing a process or a workflow. Or it might be designing a technological solution which improves system-to-system integration and interoperability. Or it could be creating a seamless user interface to make an arduous task easy for a user, regardless of their level of digital capability.
Our approach to digital service design aligns with the Government Digital Service (GDS) standard and involves the following 5 steps:
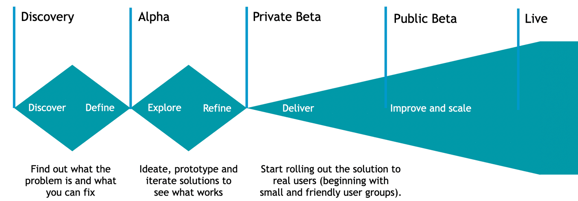
Service design is solution-agnostic. It is about deeply understanding the root causes of problems and applying design approaches to ideate potential improvements. But it does not stop there. Once ideas have been generated and prototyped, design teams test these concepts with users so that any further iterations can be made.
If you have a solution which meets the needs of the users and the organisation; and that is economically viable and technically feasible, you can progress to build. Typically, this will involve agile development to deliver incremental value at pace.
Once a solution is deployed into live, or a new process is rolled out to users, the work of the design team doesn’t stop. They scrutinise data and user insight to understand where further improvements can be made. They also seek to uncover any unintended consequences of the design intervention, so we can course-correct them. This moves you into a phase of continuous improvement, which is driven by data.
Of course, in any complex system, changing something in one area can have knock-on effects in other areas. This is why having a really deep understanding of your service through techniques like process mapping and service blueprinting enables service designers to be aware of the impacts elsewhere within the service ecosystem.
Why is digital service design so important for the NHS?
There is a lot of overlap in the way to approach service design, and the way the NHS in England has approached the creation of ICSs. Both take a systemic view - with the aim of enabling complex systems to operate more efficiently, and capitalising on those efficiencies to improve outcomes for users. Both also use evidence and data to drive decision-making.
One of the main drivers for the move to ICSs was to enable the sharing of data across and between organisations, to help decide how and where to commission services. Service design also relies on data to understand whether design interventions have had the intended impact on users of the system, and to highlight areas where further refinement is needed.
Another clear affinity between a service design approach, and the approach taken towards the development of ICSs: collaboration and partnership are the keys to success. Service design assumes that the whole is greater than the sum of its parts. It relies on participatory design and co-creation with users and stakeholders alike to ensure successful outcomes. Likewise, ICSs are striving to improve population health through working in partnership across organisational and sectoral boundaries.
An example of this is in tackling the backlog of elective care. What is needed here is a holistic, service design approach that operates at the system level. Having this high-level view makes it easier to spot where process improvements can be made, to reduce inefficiencies, increasing the capacity of clinical care providers.
This ultimately leads to the outcome of better patient care, because it means patients have a shorter waiting time. It also contributes to the reduction of health inequalities. Connecting up data at the system level enables decision-makers to prioritise those most in need of urgent care, based on their medical history or other risk factors.
In reality, service design looks different on every project. This is because no two problems look alike. In a system as complex as health and social care, there are countless dependencies, stakeholders, organisations and technologies that need to be considered. Whilst there is no one-size-fits-all model which can be applied in every scenario, service design provides tried and tested tools and techniques which can be adapted to the problem at hand.
Experienced user-centred design practitioners work as facilitators to guide you through the process of design and development. They use heuristics as well as in-depth experience of service patterns so you’re not starting from scratch when it comes to a new project.
Experienced partners for better outcomes in healthcare
Designing a new service isn’t just about creating a good user experience, it’s about designing with the user at the centre of everything you do. It also means considering a transformation from a holistic and systemic perspective. These approaches will enable the NHS to improve patient outcomes, reduce health inequalities, and increase efficiencies across the health and care system.
As organisations change from legacy to integrated, digital systems, they need an expert partner with a breadth of experience in their industry. At Mastek, we have a proven track record of delivering the healthcare experiences that patients and practitioners need. We work with your teams, enhancing your capabilities to deliver actual outcomes.
To find out how we can help your organisation with human-centred digital service design, contact us today.
How can digital service design help the NHS improve patient outcomes and reduce costs? Submit the form here to find out.
